Is Healthcare Inside Out?
In “Inside Out”, Pixar Animations 2015 blockbuster movie, we watch as 11-year old Riley, whose life to-date has been largely driven by Joy, learns the value of Sadness as she comes to grips with a life changing event. In so doing she has to let go of a piece of her childhood self but ends up a better balanced person and closer to her family.
What most movie-goers don’t know is that the story has an academic foundation in the work of, among others, Dacher Kelter, a psychology professor at the University of California Berkeley and an expert in the social functions of emotion, whose insights also have reflective implications on the practice of medicine and delivery of care.
In a 1993 paper1, Dr. Keltner and his colleagues added valuable detail to our understanding of how emotional states affect cognitive processing, specifically our appraisal of others, clarifying that “when we are angry…(others) seem lazy, manipulative, and intentionally obtuse; when we are sad we may see the very same behaviors as signs of overwork, real need, or genuine misunderstanding”
The frustration, dissatisfaction and anger of the medical community, and their perception of their well-being as threatened by system-level factors, has been the subject of much attention recently2. Considering Dr. Keltner’s research, we can see how a physician’s underlying emotional state may have adverse effects on their capacity for clinical appraisal and potentially interfere with their ability to meet societal expectations for quality of care and clinical outcomes.
In my role as Chief Medical Officer of primary care network serving exclusively complex/fragile patients, I regularly observed the “Keltner effect” in action; physicians with with the most complaints were generally angry, bitter and disappointed in their careers and the changing role and place of physicians in society. In many of these cases, a genuine listener is all that was necessary to re-orient the patient relationship and improve quality and patient satisfaction.
But what about those doctors? In truth, the foundation of successful medical practice is not the scientific method, but the willingness to truly shoulder the work of worry about another, unrelated, human being. Making space in your heart and taking on the extraordinary depth of responsibility for life-changing (and potentially life-taking) decisions for other people’s lives requires energized focus, discipline, concentration and confidence, all of which must be nurtured and cannot survive in a vacuum. Our society seems to understand the importance of this dynamic when it comes to protecting and supporting the performance of elite athletes and movie actors, but we can’t seem to make the same respectful accommodations to the critical performance of those we entrust with our health and our lives. Given our ambitious goals for healthcare quality improvement, it may be in the best interest of society to provide some level of emotional security for physicians to support their inherently intrinsic motivations to positively change people’s lives.
A recent editorial lamented the increasing prevalence of process improvement methodologies in clinical operations4. While it has been well established that evidence-based process measures can have a significant effect on utilization patterns and costs in a defined population5, we do not yet understand the variables that may amplify that performance to the next level. The question then becomes: what makes the difference between achieving a 20% reduction in hospitalizations and $68 PMPM savings based on process measures alone, and achieving 60% reduction in hospitalizations and $800 PMPM savings (all things being equal in patient complexity and fragility)? At some point, it is factors beyond evidence and engineering that will influence patient outcomes.
Keltner has also established that emotions influence interactions in relationships, where they serve to a) “help individuals know others…beliefs and intentions, b) evoke complementary and reciprocal emotions in others and c) serve as incentives or deterrents for other individuals…behavior.”3 Given the power of emotions to influence knowledge, attitudes and behavior in relationships, we need to consider how human connection and depth of patient-provider relationships may be important drivers of the Triple Aim. While we typically seek to keep emotions in check in medicine, we may want to consider a more active role for them in the design of our care delivery and value-based payment systems.
In an internal study designed to define priorities for value-based care, we discovered that more care is not necessarily better when too many different providers are involved. Our analysis revealed that when a patient is ‘connected’ to a specific primary care team at the threshold of providing 75% or more care, line item costs for primary care, testing and medications may increase, but there is a dramatic drop in overall costs, specifically around inpatient care and use of other outpatient and specialty services.
Our assessment, reinforced by Keltner’s findings, is that our capacity to achieve dramatic levels of Triple Aim performance is driven by our commitment to continuity of patient-provider relationship and some associated consequences of relationship continuity which have been referred to as “professional intimacy”.
Our model of home-based primary care makes it almost impossible to maintain traditional “professional distance” and, as such, increases the likelihood of personal connection and accountability, creating a space where patient and provider find meaning and value from each other, and, in doing so, also within themselves. Professional intimacy becomes the power driving improved regimen compliance, information sharing, collaborative care planning and the desire and motivation to achieve more in one’s life.
Professional intimacy uses the power of human connection to help us better understand each other, share emotional experiences together and “serve as incentives or deterrent for …behavior.” Under it, providers and patients remain present in each other’s lives even when they are absent from our daily schedule, and, as such, the influence of the relationship extends beyond the immediate encounter.
Professional intimacy is not the same as empathy, nor is does it necessarily require blurring of professional boundaries, but is based on both parties being fully present for each other, generating a level of closeness, confidence, and affection (a’ la Carl Rogers unconditional positive regard), and generating a new level of affinity and loyalty based on mutuality, respect and acceptance (even in the face of imperfection).
At the end of “Inside Out”, Riley and her parents each have to break through their respective defenses – for Riley, anger to the point that her feelings shut down completely; for her parents, it is the faux enthusiasm they engender to help get the family through a tough transition. Only then do they find themselves on the same side, as they embrace the sadness they share, albeit for different reasons.
Perhaps the medical community needs to have a similar catharsis. Much of the situation physicians find themselves in has been shaped by outside forces wielding their influence without any values prevailing towards their well-being. With this history in mind, resistance to change on the part of physicians may, in fact, be simply a desperate attempt to achieve some level of equilibrium, when prior trends have proven to have adverse professional risks or never sustained enough traction to warrant personal investment.
However, just like Riley, maybe it’s time healthcare professionals acknowledge to themselves their sense of loss and the sadness about how the healthcare system has changed, feelings we seem to share with our patients (albeit for different reasons); by letting go of our past expectations and embracing the shared humanity of our professional relationship, it may just allow us to find a better balance and connect in ways that revitalize our relationship and our experience of giving, and receiving, care.
1. Keltner, D, Ellsworth PC, Edwards K. Beyond Simple Pessimism: Effect of Sadness and Anger on Social Perception. J Personality and Social Psychology 1993; 64: 740-752.
2. Ariely D, Lanier WL. Disturbing Trends in Physician Burnout and Satisfaction With Work-Life Balance: Dealing With Malady Among the Nation’s Healers. Mayo Clin Proc 2015; 90: 1593-1596.
3. Keltner D, Haight J. Social Functions of Emotions at Four Levels of Analysis. Cognition and Emotion 1999; 13: 505-521.
4. Hartzband P, Goopman J. Medical Taylorism. N Engl J Med 2016; 374:106-108.
5. Javitt JC, Steinberg G, Locke T, et al. Using a Claims Data–Based Sentinel System to Improve Compliance With Clinical Guidelines: Results of a Randomized Prospective Study Am J Manag Care. 2005; 11:93-102.
TWELVE TEACHERS: Celebrating the Educators Who Helped Me Along the Way
This is not a healthcare post; it’s simply a "thank you" to 12 teachers who were especially generous with their time and spirit in my life. These were teachers who ‘got me’ during times of my life I didn’t really “get” myself, adults who were both demanding and forgiving but who were truly educators and remained so even as our relationships became professional and personal.Despite differences of age and experience, all of them were incredibly respectful of my skills and talents, and gently, but definitively help me define my own path. The individuals I have called out here are educators; this is not a list of mentors or others who have supported my career; my relationships with them is defined by their primary profession.I am extremely lucky and grateful for their presence my life.
In chronological order:
1. Mrs Gusten; First Grade PS 99, Kew Gardens NY
In first grade, I would get up from my seat in the middle of a lesson and go to the back of the room to find a book or something else of interest. Mrs. Gusten seemed to understand that I had mastered the lesson and just let me do my thing. These days I’d probably be considered disruptive and tested for ADHD. In later years I had struggles with other teachers around the issue of my learning style; having had Mrs. Gusten so early in my school life, I felt there was always a chance I would be understood.
2. Miss McLaughlin; 4th grade, Bowling Green Elementary School, Westbury NY
We moved mid-year from NYC to Westbury, so I was the “new kid” in January, middle of 4th grade. She recognized that I was in a different place in terms of the curriculum and referred me for testing; I ended up being placed in a different school in the district. While that created its own problems (being the new kid twice in a few months), it put me in a class with kids who were more ‘like me’, some of whom are my friends to this day.
3. Geri Schecter; English, WT Clarke Junior High School, WT Clarke Westbury NY
It was the 70’s and younger teachers had no problem blurring the traditional student-teacher boundaries, but Ms. Schecter was the teacher who managed this better than anyone else and the first who was genuine with her presence (other teachers took kids to hockey games, but we never really knew them as people). She was a young adult who loved language, had a creative approach to teaching and who shared her ‘real’ life without it seeming remarkable. She was the adult my high school girlfriend and I chose to come with us on a non-school-related trip to Don Imus’s radio program
4. Gerald Baden/James Muff; Shop Teachers (Ceramics/Wood; Print/Metal), WT Clarke High School, Westbury NY .
Just about my entire success as an adult has its foundation in shop class. The discipline and planning required to use power tools, make mechanical drawings (accurate to 1/32 of an inch!) and tangible skills to build things were critical success factors for medical school and my subsequent careers in medicine and management. There is a whole book to be written about shop class, but suffice to say that everything I know how to do today, I learned in shop class. Academics gave me knowledge; shop class gave me skills.
5. Barbara Lerner/Victor Jaccarino; Drama Club Faculty, WT Clarke High School, Westbury NY
The rest of the foundation of my adult life rests on my experience with the theater. I use the skills of acting every day; I can also project my conversational voice – in the most intimate manner -- to someone in the back row of a 1200 seat theater, or can move in close and penetrate someone’s personal space without threat - - a critical skill for a physician. These are the skills I learned in the theater. But more important is I completely understand the value and connection associated with story-telling and the critical nature of dialog in every aspect of human life.
6. Norman Roth, PhD, Former Professor of Mathematics, SUNY New Paltz NY
I decided to go to medical school during the December break in my sophomore year in college. I had to completely change my class schedule when I got back to school in January because I had ZERO premed requirements. I was ineligible for Calculus and I went to Dr. Roth to plead my case. He gave me chance, telling me could audit his class and, if I got 10/10 on the next five weekly quizzes, he’d do some administrative magic to get me enrolled for credit. I accepted (and met) his challenge, and ended up completely falling in love with calculus – concepts I use to this day to understand the interaction of dependent and independent variables in life….the mathematics of change. I wrote to Dr. Roth – now retired -- a few years ago and he ended up sharing with me one of his own “10 teachers” stories (he also checked his grade books, which he still had, to confirm my memory of the challenge).
7. Doug Baker, PhD, Former Dean of Students and Professor of Biology, SUNY New Paltz, NY
As a college student, I had a conflict with the Director of the Peer Counseling Center, where I was a volunteer member; the issue was escalated to the Dean of Students, Dr. Douglas Baker. We all met in Doug’s office; he defused the conflict with ease. I left with the feeling I was heard and that we definitely connected in some way. Doug was transitioning back to teaching and I ended up being his teaching assistant for a new class he was teaching called the “Biological Basis of Human Sexuality”.Despite his position in the Department of Biology, Doug’s PhD is in education, and he had taught every level from elementary through high school. He introduced me to Jerome Bruner, Bloom’s Taxonomy and ways of thinking about teaching, learning and pedagogy (and how to use a blackboard effectively). We ended up writing – and receiving! -- a NYS Research Foundation grant to study the effects of a course in human sexuality on the behavior of college students, which let me get paid to spent the summer working for him on campus. With his support I was able to secure a position teaching the same Human Sexuality course in the schools Prison Education Program, and he and I DROVE TO MISSOURI in a State car to spend a week at a course taught by William Masters and Virginia Johnson!I spent more time with Doug that just about any other teacher, or non-related adult for that matter, in my life. Every day, all day in the office we shared for two years, but also at his home with his family (for both work and play); we shared many, many meals together. During these times I learned about antiques, how to point up a stone house and how to field dress a deer (well, I watched).If the foundation of my adult life is based in shop class and the theater, the framework of the structure that sits on top of it is based on my life experience with Doug Baker.
8. Steven Shelov, MD, Former Residency Program Director, Department of Pediatrics, Albert Einstein College of Medicine/Montefiore Medical Center
While in medical school, I started my first business. I didn’t call it a business at the time, these things were just ‘outside projects’; some people at the medical school (including the then-Chair of Internal Medicine) had problems with my outside projects; it just wasn’t done back then.When I graduated and started my internship in Pediatrics, Dr. Shelov was the Residency Program Director and was incredibly supportive of my interests and enthusiasm. He joined the Board of a non-profit children’s media organization I was starting and introduced me to people in his personal network to help move the project along.A few years later, we were on a panel together at the annual meeting of the National Association for Education of Young Children. As the audience filled the room, he shared with me his personal awe at the opportunities his career had afforded him; for someone I viewed as a ‘grownup” to have that sense of humility about this own life was really important for me to hear.
9. Michael Cohen, MD Former Chairman, Department of Pediatrics, Albert Einstein College of Medicine/Montefiore Medical Center, Bronx NY
Dr. Cohen was the Chairman of Pediatrics during my time in training. So much of my career has been based on the foundation of the way he said 'yes' to my ideas, projects and energy during residency, while at the same time expecting me to sustain the highest levels of performance in the job at hand. In the last 30+ years in medicine, I have met few people who are in his former position who are as open, flexible and trusting.There were few things in my life as valuable to my young, idea-crazed, energetic self than when the Department Chair said "OK, sure, that sounds interesting
10. Carleton Chapman, MD, Former Emeritus Professor History of Medicine, Albert Einstein College of Medicine, Bronx, NY
Dr. Carleton Chapman came to Einstein after retiring as President of the Commonwealth Fund (after retiring as the Dean of Dartmouth Medical School). I believe he came to Einstein because his wife Ruth said, “You can retire Carleton, but you can’t stay home”. It would have been impossible for him to stay home anyway; he was a man of extraordinary intellectual energy.Despite the 40-year difference in our ages, we connected as colleagues; we explored the realm of ideas about healthcare, medical education, social issues, and theoretical constructs of science, learning and policy, but also theater, music, art and humanity. He shared drafts of papers and book chapters with me and spent time discussing my perspective and understanding of this work. After years in medicine, at the highest levels of the profession, he was still ‘mad as hell’, pushing and demanding productive evolution of healthcare as a species.He left Einstein the same year I left residency; age 70, he told me that one of his goals was to replicate a walk across Switzerland that he took as a young man. My entire perspective on aging is based on my time knowing Carleton.
And there are two "runners-up”:
The first runner up is Dr. Gerald Nathanson, the former Co-Chairman of the Department of Pediatrics, Albert Einstein College of Medicine/Montefiore Medical Center. At the end of my internship, I was thinking about abandoning ship and pursuing some of my very exciting outside projects. I was not especially close to Dr. Nathanson during that year, but I have a vivid memory of him taking me into his office at the North Central Bronx Hospital and sitting my down for a talk about my plans. He gently made the case for my ‘staying the course’ and investing the two years to complete a credential I would have for the rest of my life. Despite my drive to invest time and attention to my exciting outside life, what he said made sense to me; I am forever grateful for that talk because so much of who I am is tied to my professional identity as a pediatrician.
The second runner up is Dr. Maynard Makman, who was a Chairman of the Department of Molecular Pharmacology at the Albert Einstein College of Medicine, and my faculty supervisor for the Medical Student Research Program, a special program to train physician-investigators. I applied and was accepted to the program and spent the summer feeding propylthiouracil to rats and then attempting tissue analysis of their substantia nigra to see if the drug had effects on the brain.
It was quickly clear that I was a singular failure as a bench researcher. I was good at the dissecting, but terrible at the science. My notebook was chaotic, my bench discipline weak and I don’t think I once got anything resembling result from the dozens of attempts I made to actually analyze tissue. I loved the idea of science and I loved scientists, I just didn’t really DO science very well.
Dr. Makman was gracious and forgiving; he never once embarrassed me or called me out for my failures. I never returned to basic science but retained a deep appreciation and honor for those who are committed to what is can be a very unforgiving, but remarkably rewarding professional path.
Do YOU have a teacher who changed your life? Why not send them a note thanking them and letting them know they remain a part of your life.
Is Healthcare “Good to Grow”?: Rethinking Leadership Talent Acquisition
One of the greatest strengths and most vulnerable weaknesses of the American medical system is our commitment to subject matter expertise as the dominant criteria for authority and career advancement.
Healthcare has traditionally taken this approach to recruiting talent, largely based on peer-review of credentials. This served the medical community well when departmental identity and membership (driven by specific education and training criteria) were the core organizing principles of healthcare delivery; it continues to be the critical when seeking specific clinical skills or vertical subject matter expertise.
However, more often than not when healthcare organizations need ‘enterprise-level’ leadership, they mine their departmental talent pool or recruit from outside an institution based on a model of ‘similarity’ of title or organization type.
It is well established that species cannot evolve without diversity in their gene pool. If healthcare is to advance and thrive in the coming millennium, there will be a need to reconsider the entire process of recruiting and evaluating leadership talent.
Medicine is not the only realm where there is a delicate balance between talent and management in service of real-time world-class performance, yet remains one of the only industries organized in domain-based verticals. In equally complex and mission-critical non-healthcare organizations – Apple, Google, GE, Boeing, Dodge – there are horizontally organized teams that are dangerously nonexistent in healthcare organizations of similar size and complexity.
The fact is that the "credentialing" approach to healthcare leadership recruitment is major barrier to healthcare reaching its full potential. Sometimes there are non-obvious, but easily transferable and critically valuable skills and experience embedded in a non-traditional professional resume. However, experts in healthcare verticals may not have the depth of professional experience to adequately understand and evaluate ‘outside-domain’ candidates.
First, there is the issue of title parity (or lack of it). A corporate vice president may have substantially more, and far broader responsibilities than a hospital vice president. A corporate VP may be a division leader, with oversight over multiple domains (e.g., sales, technology, marketing, product management), rather than the domain specific responsibilities of most hospital VPs (e.g., service line or service domain [e.g., dietary services]).
Second, there is the risk of ‘fallacy of comprehension’, when we believe we understand something, or its value, but in reality we do not. This phenomenon is especially common in healthcare, where professional success is often based on the capacity to comprehend and assess complex situations.
However, the capacity to analyze and assess skills in one domain is not always transferable to others. Unconscious, but significant bias in candidate selection may come into play when evaluating the ‘credentials’ of non-traditional candidates.
Leadership experience in ‘operations management’, ‘product management’ and ‘business development’ are three areas in which the corporate competencies are virtually unrecognizable – but may far deeper and more valuable – than the equivalent functions in healthcare system labels. More important, healthcare executives may be completely unfamiliar with the full depth and scope of positions such a ‘general manager’, or disciplines such as ‘behavioral economics’. Entrepreneurial experience, even transitional, may have provided experiences with team leadership and corporate development that are not fully understood – and therefore devalued – by many healthcare organizations.
Many academic and professional disciplines outside of healthcare have knowledge and tools that might productively contribute to the healthcare community's goals for improving the quality of care delivered to individuals and the quality of health of populations. However, this might be done in ways that are not native to healthcare thinking or operations. The "fallacy of comprehension' then becomes a barrier to knowledge and skills transfer from outside of healthcare because they are not necessarily recognized during the candidate assessment process.
An interesting analogy can be made between healthcare leadership and orchestral performance. The world-renowned conductor and pianist Daniel Barenboim once said:
“To be a great conductor requires the ability to make people want to play, it requires the ability to animate the orchestra, to teach, to cajole, and at the same time, to learn from what you hear from good players in the orchestra. In every orchestra there is somebody that always shows you something that you haven’t quite thought of before.”
Extraordinary healthcare is symphonic – each instrument being played perfectly by a “subject matter” expert, each player playing a different line of music that, in total, creates a concordant experience for the patient. The conductor does not need to be able to play every instrument, nor even ‘lead’ the orchestra, but to envision the performance as a whole and serve an essential integrating, coordinating role. Even the most virtuoso players understand they cannot conduct and sit first chair; they respect, trust and defer to the conductor because they understand that their solo may be in their hands, but the symphony only exists in the collective effort.
Achieving consistent world-class performance in healthcare – especially for emerging operating models such as population health management – will requires a diversity of skills and experience beyond what is necessarily innate to the healthcare professional community. This will require the talent identification and recruitment process to be less about assessment of ‘credentials’ and more about being open to “something you haven’t thought of before” and exploring the potential of skills and experience from outside of healthcare to contribute to clinical, operational and financial objectives of healthcare delivery organization.
Species with limited genetic variation are less able to adapt to changing environmental conditions. Looking at healthcare are a species, we would benefit considerable if we diversify our professional and conceptual leadership DNA. This will require a critical look at our own biases in the talent acquisition process, flexibility in our process of understanding and assessing the competencies of candidates beyond formal credentials or equivalent titles and a willingness to allow our organizations and systems evolve in ways we may not envision today
Why Sentences Matter: Mining Clinical Narrative to Learn ‘Why’ and ‘How’ Things Happen
When I hear free text clinical notes referred to as ‘unstructured data’ the inherent presumption is that is it “not” something it otherwise should be, as if “structure’ is and should be the standard for all data.
The need for structure is not a problem of data, but the largely artificial limitations in our current capacity to analyze information. There are no doubts that efforts to extract discrete data elements from free text through techniques such as natural language processing (NLP) will add to the quantity of accessible data around any one patient or population. However, we diminish the humanity of our endeavors to provide care when we force clinical documentation into pick-lists and forms, and miss much larger and more powerful opportunities to understand health and healing when we try to reduce free text into something other – and much smaller -- than what it is.
Free text is content, and sometimes content can tell us much more than discrete data. In 2008, blogger and content management expert Seth Gottlieb wrote a few things about the differences between content and data on the web; his points are also quite relevant when considering the value of clinical notes in the form of dictated and transcribed discharge summaries, radiology and pathology reports, surgical and operative notes and free-text fields in clinical information systems:
- Content has a voice: it is written to communicate ideas, make a point, convince; it is personal
- Content has ownership: someone created the note, from their perspective of authorship as defined by their levels of authority and responsibility
- Content is intended for a human audience, for human senses to process
- Content has context; even the most objective content contains lexical, syntactic and semantic clues about where the reader should focus their attention, what was important and what was not.
While content may contain clues about “what” happened – drugs prescribed and discontinued, diagnoses made, symptoms observed, procedures performed – it is the narrative structure of content that allows us to understand “why and how” things happened to patients and the experience, processes and decisions made by participants in a patients care. It also can give us a sense of the person being cared for, their relationships with others and how they respond to the process of care. Given the transformational challenges facing healthcare professionals and systems of care and practice, it is now more than ever that we need to make an extra effort to make sense of the world we work within and see to understand “why and how” things happen to and around patients.
After more than a decade working around some of the best academic and commercial minds thinking about ‘unstructured medical data”, we have a good perspective on the strengths and weaknesses of current approaches to text analytics in healthcare.
Combine this with a deep understanding of the limits of structured data analytics to address the critical issues facing healthcare today, and I submit we need a Moonshot mindset around the concept of Healthcare Narrative Intelligence. Narrative Intelligence is an interdisciplinary construct that originated in the MIT Media Group and subsequently evolved by Michael Mateas, Phoebe Sengers and others. The idea behind a Healthcare Narrative Intelligence Initiative would be to develop completely new and powerful methods to make sense of our healthcare world and inform our wisdom about clinical processes and care delivery operations by analyzing patient-centered clinical notes and reports and encouraging a narrative component to clinical documentation. Healthcare Narrative Intelligence would allow us to make sense of what we see provide a deeper understanding of patient care and operations that could include but not be limited to:
- Action Selection and Decision Attribution: What was the path to a specific decision and what factors affected the final decision that was made; Do these factors have any effect on outcomes?
- Collaboration/Relational Analysis: Who was involved in these decisions, what was their relationship, what were the relationship dynamics? Would a change in relational dynamics have an effect on goal achievement or system performance?
- Goal Setting: How are goals and associated goal metrics determined?
- Semantic and Sentiment Analysis: What words were used to describe the patient and their care; Did subjective elements such as meaning and emotion effect process and outcomes?
With these as the foundation of Narrative Intelligence, methodologies such as predictive modeling, clustering and pattern recognition, and comparative analysis could contribute to an entirely new approach to developing performance benchmarks.
Analytics driven by the Healthcare Narrative Intelligence framework would not require the presence of protected health information, as the insights and subsequent derived wisdom would be focused at the level of systems, roles and interactions. Health systems, hospitals and academic medical center should come together to test these models and support the development and evolution of this next generation of analytics.
“The Uber of Healthcare?”: It’s Not About the App, It’s About The Overhead.
For a very long time, one of the most valuable business assets in New York City was a yellow cab taxi medallion. With recent value in the $1 million dollar range, ownership of the medallion was a virtual cash annuity, combined with equity growth (in 2004 medallion prices were in the mid $200,000 range and have increased in value 15% year over year in the 9 years since). As one owner once put it “it even makes money for me while I sleep”, since the cars can be ‘rented’ when the owner is off shift.
Medallion owners tend to fall into two categories: Private Practitioners and Fleet Owners. Private Practitioners own their own car, have responsibility for maintenance, gas and insurance, and tend to use the cash flow to live while allowing the medallion to appreciate over the course of their career. They then cash out as part of their retirement plan.
Fleet Owners have dozens of medallions; they lease or buy fleets of automobiles and often have their own mechanics, car washes and gas pumps. They either hire drivers as employees or, more often, ‘rent’ their cars to licensed taxi drivers who get to keep the balance of their earnings after their car and gas payments.
In London, taxi drivers have to invest 2-4 years of apprenticeship before they can take and pass a test called “The Knowledge”. However, like NY, finally getting that a licence to operate a Black Cab in London is a hard-working but stable way to earn a living.
Now imagine that someone comes along that can offer all the services of the NYC yellow cab or the London Black Cab directly to the general public, but does not have to own the medallion, own the car or employ the driver. With as much as 70% lower overhead, they provide the same service to the consumer; in fact they are so consumer friendly that they become the virtual gatekeeper for all the taxi and car service business in the community.
How, you ask? Outsourcing the overhead and just-in-time inventory management; they convince thousands of people to drive around in their own cars with the promise of a potential payment for services driving someone from point A to point B. All these drivers have to do is meet certain standards of quality and safety. This new company does all the marketing and uses technology to make the connection between the currently active drivers and those in need of a ride; they provide simple and transparent access to a host of cars circulating in your neighborhood, let you know the price and send a picture and customer rating of the driver, all before he or she arrives, and they process the payment so no money ever changes hands.
This is the premise behind Uber, a very disruptive take on the ‘taxi’ business. As a recent article in Bloomberg News noted, the slower rate of growth in medallion value is already attribute to the very young company; a recent protest by Black Cab drivers in London resulting in an eight-fold increase in Uber registrations.
Now imagine that a new healthcare services company comes to your community offering population health management services on a bundled payment or risk-basis. They guarantee otherwise inaccessible metrics of quality and safety to both large employers and individual consumers. They employ only a handful of doctors, but do not own any hospitals, imaging centers or ambulatory care facilities.
However, they are masters at consumer engagement, creating levels of affinity and loyalty usually found with consumer products and soft drinks. They use a ‘don't make me think” approach to their technology, seamlessly integrating analytics and communications platforms into their customers lives, and offer consumers without a digital footprint a host of options for communications, including access to information and services via their land lines or their cable TV box. They leverage high-level marketing analytics to determine who will be responsive to non-personal tools for engagement, like digital coaching, and who requires a human touch.
Care Planning is done based on clinical stratification and evidence; population specific data is used to determine the actual resources required to achieve clinical, quality and financial goals (a mid-West ACO has more problems with underweight than obesity, do they need to maintain their bariatric surgery center?). Physicians serve as ‘clinical intelligence officers’, creating standing orders across the entire population, implemented by non-clinical personnel; they also create criteria for escalation and de-escalation of services and resource allocation based on individual patients progress towards goals. They employ former actors and actresses as health coaches and navigators, invest heavily in home care and nurse care managers and use dieticians in local supermarkets to support lifestyle changes (while accessing and analyzing the patients point-of-purchase data to see what they are really buying).
The ‘primary relationship' between patients and their health systems is with a low cost, personal health concierge: primary care physicians who agree to standards of quality and accountability get a guarantee of traffic based on predetermined eligibility criteria and are spared administrative burdens. Multi-tiered scenario planning for emergencies is built into the system. For professional resources only required on an 'as-needed' basis, such as hospital beds, surgeons and medical specialists, access is negotiated in advance based on a formula of quality standards and best pricing but only used on a just-in-time basis (Alert: ICU bed required in 6 minutes, who wants the job?).
They are not a payer, although a professional relationship with them is on a business-to-business basis. They are a completely new type of health system, guaranteeing health and well being, transparent in their operations and choosing their 'vendors' based on their willingness and ability to achieve those goals. In doing so, they significantly reduce the resources necessary to achieve goals for quality of care and quality of health across the entire population; they treat quality achievement as an operational challenge and manage their supply chain accordingly.
Am I suggesting this a new model of care? No, I am personally an advocate for physician-driven systems of care. But this kind of system is very possible, and there are companies working on models of “national ACOs” using many of these principles.
The Uber of healthcare will have much less to do with the “mobile app”; and far more to do with creating value by minimizing overhead, designing flexible operations, supporting goal-directed innovation and bringing supply-chain discipline to the idea of resource-managed care delivery. It will involve embracing models of care delivery that leverage emerging evidence on non-clinical approaches to health status and quality improvement, and focusing on designing goal-directed interactions between people, platforms, programs and partners.
I can hear more than a few of you creating very good reasons why it wont work (“you can’t put an ICU bed out to bid!”), but these scenarios are very do-able. If we want to revitalize the experience of care for patients and professionals, we must be willing to acknowledge and embrace dramatically different, often counter-intuitive, operating models for care that will require new competencies, forms of collaboration and reengineering the roles and responsibilities of those who comprise a patients ‘health-resource community’
We Think We Can, We Think We Can….But What If We Can’t?
At one point early in my life as a physician-executive, I founded and ran an operating division of a global healthcare communications company. We were successful our first year; three years later we had more than tripled our revenue, grown to 10+ people and were contributing significant business to the parent agency
As I prepared for my annual planning meeting with the CEO, we were looking at 50% growth, adding 5 more staff and a serving as a channel for low 8-figures worth of agency revenue; the future looked bright.
On the morning of the meeting I flew in on the redeye from a client meeting in Los Angeles and went right to the office with my deck and spreadsheets; that evening I was scheduled to host an oncology-related panel of physician thought leaders at a NYC mid-town hotel.
As expected, the planning meeting included the agency CEO, divisional CEO and CFO. I started to tell a story about my trip to LA, but there was awkwardness in the room, so I paused.
….and was told the company no longer needed my services.
No harm or foul, they said, just business. They had already made arrangements for the panel that evening; everything else was taken care of as well. I was asked to leave right then; I left in a daze.
I could have found lots of things to blame: the CEO was new, he had not hired me nor been involved in the strategic thinking that created the division in the first place; my compensation package was structured in such a way so as to take significant cash off the bottom line if I hit my targets; shared clients looked to us for strategic counsel and the agency staff were relegated to subordinate roles on the team.
But I knew that day I had done something fundamentally wrong, and it took me a while to figure it out: I was unskilled and unaware of it. I may have had many successful projects and demonstrated a powerful capacity to understand, decipher and change the trajectory of complex situations, but I was not a successful leader, nor, in retrospect, did I truly understand the dynamics of the foreign ecosystems I had entered.
Having Answers is Not the Same as Having Knowledge
Smart people usually think they can figure things out, and people who are used to working on complex, multi-factorial problems even more so. But as I learned the hard way, skills mastered in one environment are not necessarily be transferable to another, and the capacity to formulate an answer is not the same as having real knowledge.
We all know the story of “The Little Engine That Could”, who, when other bigger and stronger engines reject the chance to help a train in need, digs deep down to overcome his own perceived limitations of power and skill to save the day. For decades, children (and adults) have been exposed to the “I think I can” mantra to represent the idea they can do anything if they just put their mind to it.
But what if they can’t? What do they do then?
According to a 1999 study entitled “Unskilled and Unaware of It: How Difficulties in Recognizing One's Own Incompetence Lead to Inflated Self-Assessments”, (J Pers Soc Psych. 1999 77:6) more often than not they do what I did: unconsciously miscalibrate themselves, overestimating their abilities.
This elegant paper describes four separate studies which confirm an important dynamic of personal and professional development: that individuals who are objectively incompetent (based on bottom quartile scores in tests on a range of common cognitive or subject matter specific skills) but who are unaware of their actual skill level, tend to hold overly optimistic views about themselves – and overestimate their abilities even more when they face more difficult tasks. For example, for one measure, individuals with test scores in the 12th percentile estimated their skills at the level of performance required to score at the 62nd percentile
In addition, the study found that even when faced with feedback as to their inabilities, the incompetents’ opinions of themselves largely remained unchanged. In contrast, “competent” individuals tended to underestimate their skills, were less secure in their capabilities but also optimistically – and generously -- assumed that peers shared their proficiency levels.
The bottom line: individuals may impede their own learning capacity by inflating their ‘sense of skill’; which, in turn, further inhibits their ability to recognize their own incompetence, further sustaining their potential for ‘mistaken conclusions and regrettable errors’.
There have been many reviews and critiques in the years since this has been published,, but the basic premises have held up remarkably well. Of course, no one wants to think of themselves as limited, so readers of this article tend to see the ‘incompetents’ as some form of ‘other’, (their boss, their colleagues, their competitors), but, in fact, the conclusions also hold up when considering individuals who demonstrate intelligence and skills in other areas. In fact the authors found that the tendency of people to overestimate themselves is linked to some internal threshold of ‘knowledge, theory, or experience that suggests to them that they can generate correct answers’. (Once again proving that a little knowledge is a dangerous thing).
The true take-away from this article is that we should worry more when we (think) we know what to do, and less about the competence of those around us. Fortunately for us all – and as I discovered in my own quest - when actively trained, people better understand the limits of their abilities and recalibrate their self-assessment to better align with their actual skills levels.
What happens to those who are ‘unskilled and unaware”? They persist, but they do not evolve, risking extinction. Kind of like our current health system.
This came to me recently during a meeting with a prospective hospital ACO client, who was struggling with “patient engagement.” (more specifically allocation of capital against engagement). Their efforts were grounded in two approaches: their EHR patient portal and a call center, staffed by nurses. But response rates were low, and actual ‘engagement’ – meaning interaction towards a goal -- was even lower.
With my background in communications, I asked some questions about message testing and customer segmentation. These concepts were unfamiliar to the clinical and administrative leadership (no one from marketing was in the room), however, received with great enthusiasm. Some very bright people were putting substantial time and attention against this problem and were simply unaware of methodologies that, until recently, would otherwise have been irrelevant to their careers. It started me thinking: in what other areas might healthcare as a whole be ‘unskilled and unaware”?
My sense is that in healthcare, when faced with tough problems, we think we can figure them out. Inflated self-assessment is as much a cultural phenomenon as an individual one; not only do we miscalibate our own skills, but we collectively inflate our capabilities as a community.
This is particularly relevant as the healthcare community at large attempts to embrace “population management”. As its foundation, population management requires implementing and mastering a separate and distinct operating model from traditional care delivery, including a specialized infrastructure with its own functional requirements and the capacity to orchestrate and optimize goal-directed collaboration and operating relationships among the people, programs, platforms and partners that make up that infrastructure.
Designing and executing on this requires knowledge, skills and competencies that are at best peripheral to healthcare and unlikely to be part of the knowledge base of health professionals or administrators. Systems design, analytics, customer segmentation, modeling and targeting, consumer engagement, behavior change, resource management and operations efficiency all have relevant and well proven solutions from outside of medicine yet at hospital after hospital, teams of people are investing hours of brain-power trying to ‘solve’ these problems (or relying on vendors who come to the table with categorical answers but expect the clients to manage the system-level context of their offerings). More often than not, the knowledge necessary is just outside the door.
While lifelong learning is a characteristic of healthcare professionals, this learning tends to be focused on matters external to the profession itself – science, patient care and other categorical subject matter. While it may seem extreme for me to say, in my 30 years experience, when healthcare does seek new knowledge, we tend to look within the four walls of the ‘house of medicine’ and sometimes assumes that if we cannot find the necessary answers there, they do not exist. I have also experienced situations where, when there was some indication of relevant knowledge, theory or experience in a problem area from outside of medicine, its value was diminished or dismissed as not having been studied with sufficient rigor to be trusted.
Evolutionary forces have presented us with some challenges; we have some new things to learn. Why try and figure it out ourselves? What can we learn from jazz musicians about how to collaborate for high-level performance? What can we learn from the oil industry about balancing resource allocation with care plan performance goals? What can the payers teach us about risk profiling? Can cable TV set top boxes be employed to collect health risk assessment data? What can credit cards teach us about customer loyalty and steerage? Could we design different CAD interventions if we had the “point of sale” data collected by supermarkets?
In his 1978 book, Behind the Mirror: the Search for the Natural History of Human Knowledge, Nobel Prize winning ethologist Konrad Lorenz, describes evolution as a process rooted in interaction with – and perception of -- the outer world. Drawing from his research with animals in the natural environment, Lorenz describes how organisms use information to advance their effectiveness. Lorenz considers “exploratory behavior” as a mark of the developing organisms and species (think fish who try and leave the pond, thousands may have tried and failed but the one who made it started something big) and highlights ‘learning after maturity’ in particular as an important evolutionary advantage (hence our brains developing consciousness to the disadvantage of our once massive musculoskeletal systems).
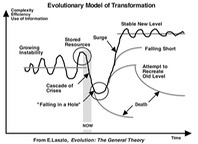
However, medicine is often unconsciously considered by its members to be a “mature species” – resulting in little exploratory behavior and associated ‘learning after maturity’ as a profession. When combined with a track record of miscalibrating our own skills when faced with new challenges, it is little wonder that healthcare is being buffeted by external forces and struggling to make progress in its evolutionary path. In fact, the forces of maturity are so strong, that, when stressed, healthcare (as a species) makes desperate attempts to achieve equilibrium -- when equilibrium is impossible and change is unavoidable – resulting in further marginalization from the evolutionary progress.
One of the greatest strengths and most vulnerable weaknesses of the American medical system is our commitment to subject matter expertise as the dominant criteria for authority and career advancement. The fact is that mastering a complex subject and achieving thought leadership status in a subject-specific field does not automatically make someone capable of solving equally complex problems in an unrelated field; they may understand the problem and generate answers, but do not necessarily have the knowledge necessary for optimal operational problem solving.
While there has been some demonstrable movement towards embracing ‘knowledge transfer” from other discipline (e.g, Lean and Six Sigma frameworks, quality practices from the aerospace industry and others), this approach is not normative (which historically will confer evolutionary advantage to some). As well, when some new ideas are considered, they are usually considered in the context of a specific problem (e.g., quality) or in support of a status quo objective.
The key to shifting our current evolutionary dynamic is for everyone to understand that future healthcare is going to require systems (and associated capabilities and competencies) with which the current healthcare community has very limited experience and even, in some cases, no real frame of reference. Evolution of our roles and responsibilities is inevitable and the more we explore the ‘outside world’ for models and solutions to integrate and adopt as our own, the more likely we are to make magical discoveries and support our own advancement and prosperity as a community and as professionals.
The Future of Hospitals: Not BUH-Bye, but B2B
In 1950, business life looked good for the US Railroad system. With almost 100 years of dominance of the American transportation system, the US railroad system had 7 times the intercity passenger-mile traffic of the then-30-year-oldcommercial airline industry.
However, by 1970 the tables had turned, with airline service carrying passengers then 9 miles for every mile traveled by rail services, which ended up bankrupt and nationalized. (Interestingly, the proportion of passenger traffic maintained by inner city buses during this time changed very little).
While many forces drove this change – the Interstate Highway System, the familiarity and comfort of returning WWII veterans with airplane travel, and shifts in mail sorting technology were all factors -- one of the biggest failures of the railroad industry itself was the way they defined themselves.
By not envisioning themselves as being in the transportation business, railroad executives created an artificial isolating barrier where airplanes were outside their operational frame of reference, and, in fact, ignored as a potential threat to their survival. If the railroads had decided to categorize themselves as being in the ‘transportation industry’, they could have invested in airlines and modified their rail service strategies based on market forces, allowing a more productive evolution, but hubris and legacy blinded them to the reality of social dynamics.
This phenomenon was largely repeated when the Internet emerged as a competitor to the print publishing industry and looms prominently in the future of the inpatient hospital industry.
As one historical reference on rail transformation notes: “An entire generation of rail managers had been trained to operate under (a restrictive) regulatory regime…Labor and their work rules were likewise a formidable barrier to change.”
Which could be rewritten thus: “An entire generation of healthcare administrators had been trained to operate under an increasingly restrictive fee-for-service model. Physicians and the existing operating model for care delivery were likewise formidable barriers to change”
Reducing preventable primary and secondary hospitalization rates in a defined population is a well-proven competency for health plans (and their “Plan Sponsors”, usually self-insured employers); their financial incentives are aligned to do so (they get to keep any unspent money), and by and large, their success is driven by
- Improvements in the quality of care delivered to covered patient-employees (e.g., closing evidence-based gaps in care and focusing on clinical risk-reduction strategies) and
- Targeted shifts in patterns of resource utilization and patient engagement (introducing Care Management for example).
While the absolute levels of engagement and quality improvement by Health Plans is quite low (only closing 26% of identified gaps in care in one study; only reaching 13% of patients eligible for Care Management in another), the results still have been quite dramatic; a 9% reduction in hospitalization rates can save (tens of) millions of dollars; shifting emergency department utilization via telephonic and urgent care is both financially and operationally valuable under risk- or bundled payments models.
“Accountable care” shifts in the locus of control (and costs) of these care delivery strategies from the employer to the provider. However, as the health plans know very well, when the patients physician recommends care management, engagement and compliance levels rise, raising the potential for successful prevention of the ‘most impactable hospitalizations’ under the population health model. Combine this with “bundled payments” or "capitation+ bonus”, or full risk, there is an incentive for more intensive resource (cost) management by providers by sourcing and using lower cost/high efficacy tools and interventions.
When in the business life of a value-based health system does it stop making sense to own an inpatient facility? What happens when the costs of inpatient services are ‘out of its own pocket’ and do not have any direct associated revenue? How do value-based health systems make the determination as to which resources to own and which to contract for on an “as-needed” basis?
Another problem with the railroad industry (and the print publishers as well) is that even when there was a recognition that things were changing, there was a concerted effort to shape the change to retain the status quo. I once heard a publisher whose magazine was getting thinner and thinner every month, say “We’ll give away web banner ads in order to sell more print pages”. On the surface, 15 full-page ads at $20,000 does not have the same value as 3,000,000 ad impressions at $25 per 1000. The real problem was that his P&L had to pay for the print production infrastructure. The print margins were 15%, leaving $45,000 in profit on $300,000 in revenue; the web margins were 45%, leaving $33,750 profit on $75,000 in revenue. Divesting the print production infrastructure and leveraging the subscriber list to build web traffic would have resulted in lower revenue, but much higher profit venture -- as many newspapers and magazines eventually figured out often too late to maintain their market share.
With the gradual decline in healthcare fee-for-service revenue will come an associated sea change in the concept of “return on investment” (ROI). First, the administrative infrastructure for coding and billing will no longer be necessary, although some of the coding functions can be repurposed for clinical and operational analytics. No longer will the value of an infrastructure or resource-related expense be assessed on its dollar-for-dollar return. In value-based care, ROI calculations will have to be determined under an operational efficiency model. Performance consistency, flexible operations, clinical supply chain management and customer value will become new standards of health system operations.
The questions a CFO will have to ask are:
- What is the cost/efficiency value of a resource to my ability to meet my contractual goals for quality, efficiency and patient experience management?
- What is the portfolio of resources I need to deploy in order to meet those goals in the most efficient (highest effect/lowest cost) way possible?
- What are the criteria I need to escalate and de-escalate resource allocation with any individual patient (taking into account individual patient attributes, preferences, and goals)?
- When I must deploy significant or complex portfolios of resources against a patient (e.g., emergencies, exacerbations of existing conditions), do I need to own them, or can I use a ‘just-in-time’ inventory construct and contract for them “on-demand”?
- When I do contract for on-demand care delivery services, how can I assure those vendors (which may include inpatient services, imaging and medical and surgical specialists) will be accountable for their contribution to my contractual goals for quality, efficiency and patient experience management?
Today's hybrid fee-for-service + gainshare or 'pay for performance' models are offering a transition window of economic comfort to health systems. But as cost-shifting gets more traction, eventually there will be a tipping point where, even with a successful effort at “steerage” – assuring patients stay within the ‘network of accountability’, it will take great economies of scale – tens or hundred of thousands of patients – to generate enough inpatient volume to justify a health system retaining its hospital. The likelihood of any one ACO succeeding with the cost of an inpatient infrastructure on the books is very low. Why keep the building and staff on the books when you can divest it and competitively negotiate terms and rates?
The same is true, by the way, for specialty services; the only ones an ACO might want to invest in will be driven by the population analytics. One ACO I work with has no need for a bariatric obesity program because the vast majority of their population is underweight; while analytics may justify primary care and certain specialties 'on staff' there will be an entirely new forms of private practice for specialties where services are provided to system-attributed populations, not geographic communities.
The economics of ‘accountable care’ will naturally lead to a divesture (or abandonment) of the infrastructure and overhead costs associated with running inpatient services, some high cost imaging services whose success was based on fee-for-service ROI models, and some specialty services with limited 'need' in an attributed population. Since the population health model is also based on keeping patients in the ‘network’, hospitals (and some specialists) will not compete for share of mind of patients, but share of market from ACO’s.
The future of the inpatient hospital will be as a freestanding ‘on-demand’ service competing for business-to-business contract with value-based system of care under a population health management model (interestingly this is similar to what health plans do today). Even when an inpatient hospital and an ACO are under part of the same corporate parent, it will increasingly be a zero-sum game to have the profitable ACO offset the losses or required investment of the inpatient service; the hospital will have to become ‘market competitive’, wooing and negotiating with a all the local “ACO’s” to provide value-driven services at competitive levels of quality and cost
Can Medicine Learn from Art History?
 David Galenson is a world-class economic researcher and professor at the University of Chicago, who also happens to have deep interest in the process of innovation. In his book "Conceptual Revolutions in Twentieth Century Art", Dr. Galenson applied some of his substantial research skills to art history and the phenomenon of creative change; there are whole parts of the book in which I could have just crossed out "art" or "artist" and "20th century" replaced them with the words "medicine", "physician" and "21st century" and the points would be equally valid and powerful. This is especially true when examining acceptance of innovation, the role and influence of peers in managing creative change and the issue of 'rate of change'; below are a few excerpts from the book, along with my parallel thoughts with regard to the world of healthcare…..
David Galenson is a world-class economic researcher and professor at the University of Chicago, who also happens to have deep interest in the process of innovation. In his book "Conceptual Revolutions in Twentieth Century Art", Dr. Galenson applied some of his substantial research skills to art history and the phenomenon of creative change; there are whole parts of the book in which I could have just crossed out "art" or "artist" and "20th century" replaced them with the words "medicine", "physician" and "21st century" and the points would be equally valid and powerful. This is especially true when examining acceptance of innovation, the role and influence of peers in managing creative change and the issue of 'rate of change'; below are a few excerpts from the book, along with my parallel thoughts with regard to the world of healthcare…..
”Innovation has always been the distinguishing feature of important art, but the need for innovation to be conspicuous is a particular hallmark of the modern era, and the pace of change has accelerated within that era.”

We all know the quoted studies on how it takes 20, 30 years for valid research findings to become accepted as standards of care, but in today's healthcare, the phenemenon of innovation extends beyond considerations of diagnosis and treatment to the very nature of the profession, roles, responsibilites, relationships, models of collaboration and tool sets. And the demands on individuals and systems to change have become intense. This was also the case in the transition in art in the early 20th century; for decades, stylistic change was glacial, "movements" were well established. Before 20th Century art, a painter of Picasso's power and influence would never have changed style; yet change was Picasso's raison d'etre. Today, in healthcare we see lots of forced change under the guise of innovation. It will be interesting to see which of those changes will constitute "true" innovations with lasting affect. Of course, the art world didnt have a multi-billion dollar Federal program pushing one form of innovation over many others, but, as I have said before, evolution in this regard cannot be stopped. As to whether innovation can be forced, Galenson's opinion can be summed up in this quote:
“In 1965, Harold Rosenberg, who was himself a leading critic, conceded that “Manipulated fame exists, of course, in the art world.” Yet he emphasized that this fame was fleeting: “The sum of it is that no dealer, curator, buyer, critic or any existing combination of these, can be depended upon to produce a reputation that is more than a momentary flurry.” Real power in the art world came from only one source: “the single most potent force in the art world is still, in the last analysis, the artist . . . “
 Many of us see the current vision of EHR's and meaningful use as being "momentary flurry". The question then becomes, however, what will remain or what will evolve, if, to paraphase Galenson, "the single most potent force in healthcare is still, in the last analysis, the physician" And long these lines, Galenson noted:
Many of us see the current vision of EHR's and meaningful use as being "momentary flurry". The question then becomes, however, what will remain or what will evolve, if, to paraphase Galenson, "the single most potent force in healthcare is still, in the last analysis, the physician" And long these lines, Galenson noted:
“Important artists are innovators whose work changes the practices of their successors. The greater the changes, the greater the artist. It is those artists who have the greatest influence on their peers – and the artists of later generations – whose work hangs in major museums, becomes the subject of study by scholars, and sells for the highest prices.” “Perhaps the importance that we must attach to the achievement of an artist or a group of artists may properly be measured by the answer to the following question: Have they so wrought that it will be impossible henceforth, for those who follow, ever again to act as if they had not existed?”

True in medicine up to a point: names like Semmelweis, Lister, Pasteur; Olser, Salk, Penfield, Freud all fit the criteria. But we have lost, or fragmented, the idea of influencers at these levels; these days innovation, if it happens at all, happens within specialties, not across the overall 'professional identity' of physicians as a class. Who among our peers today is doing work that will forever change the way we think about medicine? Have we restricted our growth as a profession by limiting the innovation paths between and across disciplinary boundaries? And how do we treat our innovators?
“Significant artistic innovators are of course not simply initially unappreciated: they are vigorously attacked. Any innovative new art form necessarily involves the rejection of older values. For practitioners and admirers of those older values, this causes “a sense of loss, of sudden exile, of something willfully denied . . . a feeling that one’s accumulated culture or experience is hopelessly devalued.” It is hardly surprising that those committed to established forms refuse to accept innovations that would make those forms obsolete, and thus cause a devaluation of their own knowledge and skills. This phenomenon is not unique to art, but in scholarship is known as Planck’s principle, named for the physicist Max Planck, who observed that “a new scientific truth does not triumph by convincing its opponents and making them see the light, but rather because its opponents eventually die, and a new generation grows up that is familiar with it.”
I hope Plancks sentiment is not true, but I have unfortunately experienced the vociferous Kubler-Rossian anger of my peers (my peers!) because of something as simple as an unexpected demand on their intellectual attention; the very existance of threats to 'retire' due to changes in form and function of the practice of medicine is a sad commentary on the lack of capacity of whole generations to organically evolve their professional identity and take entrenched reactionary positions.

“Examples of great artists who evolved from youthful revolutionaries into aging reactionaries are not difficult to find. Leo Castelli opened an art gallery in New York in 1957, and only a year later presented Jasper Johns’ first one-man exhibition, which was an immediate sensation in the art world. Castelli became the leading art dealer of the 1960s and 1970s, representing Johns, Robert Rauschenberg, the major Pop artists – notably Andy Warhol, Roy Lichtenstein, and Claes Oldenburg – as well as such younger stars as Frank Stella, Richard Serra, and Bruce Nauman. In an interview in 1994, Castelli recalled his dismay when the 1993 Whitney Biennial exhibition had forced him to recognize the impact of new developments that had been occurring in advanced art, with the increased use of new media, including video, and the prominence of younger German and Italian painters: “I had to accept the fact that the wonderful days of the era I had participated in, and in which I had played a substantial role, were over.” He initially could not accept the legitimacy of the newer art: “I felt that what had been there before, during the great era of the sixties, was unbeatable, and that nothing of that kind could succeed the heroic times that we had had here in New York.” On reflection, however, he realized that he had to accept the new art, so that he would not repeat the universal error of aging art experts: “There was a certain sadness that I felt about it, but well, with the Whitney show, I realized that I had to change my attitude, and not be rejecting – as people generally are, as you know. I would say that there is a span, a relatively short span, in which somebody really lives seriously with a period of art and after that, all those people – whether it be dealers or art historians or museum directors – after that they don’t see what’s going on anymore. They reject whatever comes after that. I didn’t want to be one of those.”

In my mind I am still an 'early career' physician (and I still should wear size 32 pants), but I did find myself recently telling a "when I was your age" story to some genuinely early career physicians about what life was like being on call for 36+ hours straight every third night. And despite whatever objective criteria were the basis of such changes in residency training, at a very basic level I believe there was something significant lost in the transition. Comparing my experience to theirs, I completely understand what Castelli was saying when he felt that "what had been there…was unbeatable, and nothing of the kind could succeed the heroic times we had". However, I am an unrepentant career chameleon, so real my worry is that such a deep, left brain response to innovation by a entire (and vitally important) generation or two of physicians is going to hold back the ability of our profession to see the opportunity in front of them to recapture/reengineer our leadership role in the healthcare system

“Significant innovations inevitably impose losses on those who cherish the values the new innovations reject, but of course they also offer gains. The artistic innovators who are faced with attacks on their new methods understand this. For example, Kazimir Malevich remarked in 1919 that “People always demand that art be comprehensible, but they never demand of themselves that they adapt themselves to comprehension.” When artists create significant new forms of art, they almost invariably see their innovations denounced by critics who are judging their new methods by the rules or conventions of earlier art, which the innovators have intentionally discarded. Thus in 1914, Wassily Kandinsky warned against critics who claimed to have found flaws in new art: “one should never trust a theoretician (art historian, critic, etc.) who asserts that he has discovered some objective mistake in a work.” Kandinsky explained that, in ignorance of the purpose of the new work, the detractor was invariably applying outmoded criteria: “The only thing a theoretician is justified in asserting is that he does not yet know this or that method. If in praising or condemning a work theoreticians start from an analysis of already existing forms, they are most dangerously misleading.” Ideally a critic would take care to understand the new methods of the innovative new work, then explain it to a wider audience: “he would try to feel how this or that form works internally, and then he would convey his total experience vividly to the public.”

And this is even worse with physicians, who are cognitively trained and culturally oriented to finding pathology. You cannot get in front of a group of doctors with a new idea -- even one with gobs of rational scientific data behind it -- and expect it to be accepted. They are compelled to poke, prod, dissect and otherwise deconstruct it to find the flaws. And they approach every problem with the presumption that whatever is seen on the surface is hiding some weakness or imperfection; because the worst thing a physician can do is miss something that is wrong. There is an additional problem when they are asked to evaluate or assess the value of something that is based on principles with which they are unfamiliar; rather than say "gee, help me understand how this works", they make analogies to the familiar and allow those "outmoded criteria" to run their judgement.
“Yet the difficulty of understanding innovative new art has increased over the course of the modern era, because of the increasing prominence of highly conceptual art. Understanding advanced art would subsequently be primarily intellectual rather than visual: “An advanced painting of this century inevitably gives rise in the spectator to a conflict between his eye and his mind; as Thomas Hess has pointed out, the fable of the emperor’s new clothes is echoed at the birth of every modernist art movement. If work in a new mode is to be accepted, the eye/mind conflict must be resolved in favor of the mind; that is, of the language absorbed into the work.”
I'll let Picasso take this one: “The fact that for a long time cubism has not been understood and that even today there are people who cannot see anything in it, means nothing. I do not read English; an English book is a blank book to me. (But) this does not mean that the English language does not exist. Why should I blame anybody else but myself if I cannot understand what I know nothing about?”

The future of medicine lies in our ability and willingness to absorb and be changed by new ideas.
“In part, the difficulty at issue here is simply that of assimilating innovative new art in a period of rapid change"
"In part, the difficulty at issue here is simply that of assimilating innovative [new approaches to the art of medicine] in a period of rapid change."
More on how we can accomplish this in the next set of posts.
What it is!..and what it will be….

I read with dismay a recent announcement that as many as 34% of American physicians are considering leaving the profession in the next 10 years, and 16% will make some transition away from clinical practice in the next 12 months; remarkably similar data were also published in 2010 in the New England Journal of Medicine.
Both surveys came to the same conclusions: physicians are unhappy about their professional lives, and are extremely pessimistic about their futures. While economic burdens – costs more than income – are cited as a top reason, the bulk of their concerns related to their sense of control – or lack of it – over their professional identity and the role and place of physicians in emerging systems of care.

However, we are now at a moment in history where there is an extraordinary opportunity for physicians to recapture their leadership roles in patient care and the systems of care in which it takes place. If the operational systems and technology that are being imposed on us are flawed and less than optimal in design and functionality, that means there is an opportunity to actively determine the fate of what is likely to be an ‘intermediate species’ in the evolution of modern healthcare, and the professional of medicine has an incredibly powerful tool that we can, and must, employ to wrest control and drive the evolution of these systems: science.
So, please friends and colleagues: don’t go yet, the biggest opportunity of our careers is just opening up.
Medicine is the science of solving human problems, and success requires mastery of science, problem solving and humanness. We trusted in this model to give us the power to care for patients and we must trust in it to help us revitalize our roles as leaders in the healthcare system. A recent report issued by The Physicians Foundation spelled out our value very clearly: “Physicians and their relationship with patients constitute the animating principle of the US healthcare system”
Unfortunately, for most physicians today, the environments in which they work, whether in independent private practice or as organizational employees, are killing this vital spirit and undermining the very contribution physicians are expected to make to the success of the system. One of the fundamental requirements of the successful practice of medicine is the sense that your efforts – your studies, your discipline, your mastery, and your work of worry -- will be channeled to achieve some form of positive results for your patient and be valued by the community.
Health professionals take on an extraordinary depth of responsibility for other people’s lives; as
such, their confidence, optimism and professionalism must  be nurtured and cannot
survive in a vacuum. Our society seems
to understand the importance of this dynamic when it comes to the performance
of elite athletes, but we can’t seem to make the same respectful accommodations
to the critical performance of those we entrust with our health and our lives. But while “the system” today may not
adequately support the role of physician as central figure, an emerging set of
critical issues will place physicians, if we are organized enough to take advantage
of it, in a position of not only controlling our own destiny, but driving the
fundamental framework for “the system” itself.
be nurtured and cannot
survive in a vacuum. Our society seems
to understand the importance of this dynamic when it comes to the performance
of elite athletes, but we can’t seem to make the same respectful accommodations
to the critical performance of those we entrust with our health and our lives. But while “the system” today may not
adequately support the role of physician as central figure, an emerging set of
critical issues will place physicians, if we are organized enough to take advantage
of it, in a position of not only controlling our own destiny, but driving the
fundamental framework for “the system” itself.

Once upon a time, there were well defined, socially accepted modes of interaction between patients, health care professionals, and healthcare institutions. At a superficial level, patients accepted physician authority without question and in exchange, physicians would shoulder the whole work of worry about a patient’s health; while this model had its own flaws, it left the social structure of healthcare more certain. It was from this social compact – a balance of singular authority and mutual commitment — that patients felt they were able to move through difficult times with confidence.
While the paternalism of the old model is largely unacceptable in modern society, the model had a sense of wholeness and integrity that was comfortable and comforting to patients and community, providing a central figure — the physician — who accepted us in the face of imperfection, offering a professional form of unconditional love and its associated commitments.
Patients and the community are now
confronted with increasingly complex systems that are iterations of adaptations
to situations and circumstances – many of which began outside the realm of the
healthcare system – and often find themselves stranded without credible social
constructs for healthcare, often with fluctuating authority. The deconstruction of the culturally standardized healthcare structure has left us with a system that has no
rational base. The system has no evolutionary logic, nor could it pass even the
most superficial test of ‘evidence-based’.
standardized healthcare structure has left us with a system that has no
rational base. The system has no evolutionary logic, nor could it pass even the
most superficial test of ‘evidence-based’.
As a result, most people face major healthcare events with doubt and confusion.
Deconstruction of physician authority may have brought about broader individual awareness, but also systemic weaknesses; the physician community, vulnerable to competition for our social capital from forces who were unimpeded by the mores of academic and professional fairness that underlie our profession, fell victim to those with less selfless and less generous agendas, resulting in devaluation of our role.

Physicians started out the 21st century in a position of weakness; our leadership position was weakened, our professional judgment and competence questioned and our autonomy was under threat. The “health system” showed little interest in improving medical practice and took advantage of our vulnerability by offloading administrative responsibilities and offsetting costs to the physician community.

Over time, the ‘medical-business’ complex became a superficially dominant force, and we responded by organizing around our specialty identities and entering into a zero-sum game, where we bickered over how dollars are divided among ourselves while third-parties doled them out like parents deciding if we earned our allowance; this fragmentation, pitting physician-against-physician only served to weaken the profession even more as we tried to play a game whose rules were largely foreign to our professional culture, leaving us both unprepared and ambivalent.
Professional devaluation takes place on two levels: economic and social. For decades, physicians have reacted by been trying to fight the battle on someone else’s terms – economics – and trying to fight on other peoples terms is almost always a losing proposition. The key to our success is to shift the battlefield to one in which we dominate: the science of solving human problems.
 Why go into battle at all? Why not just quit; take our toys and go
home or give up on autonomy and become salaried employees? Well, first because of why we
became physicians in the first place:
our commitment to excellence and human service, and second, because,
actually, have a good chance of winning, both socially and economically. Society needs us, and we can do
well by doing good.
Why go into battle at all? Why not just quit; take our toys and go
home or give up on autonomy and become salaried employees? Well, first because of why we
became physicians in the first place:
our commitment to excellence and human service, and second, because,
actually, have a good chance of winning, both socially and economically. Society needs us, and we can do
well by doing good.
Two forces are in our favor. The first is the evolutionary
principle, as described by Nobel laureate Edmund O. Wilson that “while within groups,
selfish individuals beat altruistic individuals, groups of altruists (consistently) beat
groups of selfish  individuals”[1]. This means that if we organize around
and commit to our fundamentally altruistic professional mission, we will have a
better chance of winning the battle for our professional identity than if we
keep trying to compete on relatively selfish goals – like money.
individuals”[1]. This means that if we organize around
and commit to our fundamentally altruistic professional mission, we will have a
better chance of winning the battle for our professional identity than if we
keep trying to compete on relatively selfish goals – like money.
The second force in our favor is the free market. It is well
established that people will pay a premium for the delivery (and sometimes just the perception) of value; the
Ford Taurus you rent from Avis is exactly the same car you can get from Budget,
yet people show preferences and are  willing to pay a premium for one over the
other. By regaining control over
our professional identity, we also revalue ourselves in the marketplace.
willing to pay a premium for one over the
other. By regaining control over
our professional identity, we also revalue ourselves in the marketplace.
This defines our mission: revitalizing the value of the physician in the healthcare system. Rather than deploy our resources across multiple battlefields, we as a profession need to rally around a singular decisive infection point: redefining the foundational role of the physician, independent but inclusive of any and all specialty perspectives or competencies – medical, surgical, behavioral -- and reclaiming our profession.

Future of physicians is actually in a modern reclamation of three traditional roles:
- The determination of the value and significance of available information and how it should be applied to or removed from decisions – and actions -- that can affect the lives of human beings
- Serving as the orchestration point for plans of care by members of a patients’ professional and personal resource-communitie
- Take responsibility and shoulder the “work of worry” for the health and well being of our entire practice population, not just those who self-select for care but those who may have been in our waiting room recently.
There was a
time when physicians shouldered all the risk for patient care; we took care of
the patient and they either paid or they did not; if not, sometimes we took a
chicken. There was also a time
when physicians were the primary employers of nurses, who served critical roles
as care coordinators and care managers.
Physicians with better reputations garnered higher fees -- of course in
those days, patient satisfaction was not scored by Federal survey, but by how
neighbors talked about you in the supermarket. This is not a call to recover the past, but to remember that
our profession is familiar with some of these principles seemingly being
imposed on us.
So, at a
moment in the history of medicine when we are needed most to achieve the
broadest improvements in the health of our nation, it is time to activate ourselves. Let us: 
- Take a critical look at boundaries to a cohesive professional identity across medicine -- the things that evolved as defensive reactions to outside threats and, if they do not serve our vision for the future, bravely eliminate them.
- Adopt the emerging roles that suit our profession – knowledge manager, population view and conductor, and find the most relevant science to support our success in these roles.
- Wrest control of the strategies and frameworks for care delivery and determinations of quality that are infiltrating our professional lives, and set the standards against which products and systems are designed and operated.
 Let us reclaim our professional identity; let's lead with craftsmanship and relentless intellectual energy and the vigorous commitment to research and discovery that is the foundation of the profession to
which we aspired. The opportunity
exists for us to rewrite the script for our future and, in doing so, define our
leadership position and value to society.
Let us reclaim our professional identity; let's lead with craftsmanship and relentless intellectual energy and the vigorous commitment to research and discovery that is the foundation of the profession to
which we aspired. The opportunity
exists for us to rewrite the script for our future and, in doing so, define our
leadership position and value to society.
Healthcare Is Not Like Flying an Airplane

TO my mind, current technologies like the EHR are really just intermediate species in the evolution of healthcare IT. The current generation of clinical technology will be likely be replaced by complex interactive computing power that focuses less on individual encounters but reflects patterns embedded in the patients data stream.

With this in mind, the way we think about technology will also have to change: goal-directed collaborations between humans and their technologic instruments will require a completely new approach to interaction design -- on that focuses less on the data and more on the meaning and value of the data to the actors in the system: patients and professionals. Part of this change will mean a shift of attention from any single category of variables to the relationships between variables – including the human factors.
 When we hear about human factors in healthcare, it is often in the context of patient safety, as in "we need to protect patients from human factors". The success and safety record of the aerospace industry is often cited in this context. But while some tasks can and should be supported by technology, healthcare and healing can only be accomplished in a human context. From this perspective, analogies between healthcare and aerospace start to weaken. Yes, we can learn some things from aerospace in terms of anticipating and preventing problems on repeatable pathways, but managing humans to optimize their quality of life is not like assuring an airplane will not crash. Healthcare technology needs to be designed to support the human factors that create quality and optimize outcomes, such as the ability to make meaning, find context in complexity, and make genuine connections.
When we hear about human factors in healthcare, it is often in the context of patient safety, as in "we need to protect patients from human factors". The success and safety record of the aerospace industry is often cited in this context. But while some tasks can and should be supported by technology, healthcare and healing can only be accomplished in a human context. From this perspective, analogies between healthcare and aerospace start to weaken. Yes, we can learn some things from aerospace in terms of anticipating and preventing problems on repeatable pathways, but managing humans to optimize their quality of life is not like assuring an airplane will not crash. Healthcare technology needs to be designed to support the human factors that create quality and optimize outcomes, such as the ability to make meaning, find context in complexity, and make genuine connections.
And since we know right brain factors like tone and tenor are sometimes more powerful influencers than logic, we may need to reconsider how healthcare is organized and delivered. This is especially important as the roles and responsibilities across a patients 'health resource-community' are reengineered, and will require more collaboration and cooperation. Patient-centered care means more than everyone facing the patient and performing their roles; interactions between the players is as important as the performance of any one player.
With this in mind, we may want to look to a performance model that has proven its ability to support masterful players, individually and in concert: the symphony orchestra.

In which dozens of technical experts, each of whom has invested years mastering their specific instrument, come together, subsume their individual identities towards concordance and together are able to move people in ways that healthcare professionals can only dream about.
Extraordinary healthcare can be truly symphonic. In the symphony,
performers use their instruments to express their part of a score to
create a harmonious experience for the audience. In healthcare, the
score is represented by the evidence and best practices, but as the best musicians know, despite the score being the same, a symphony is never played the same way twice. Healthcare players can transcend the score by being mindful of the patient and of each other,
because the symphony only exists in the collective effort.

The bottom line: Just as musical instruments cannot play themselves, healthcare technologies should be instruments of human expression in service of health and healing, with a fundamental mission to provide the patient and their family a sense of harmony and tone even in the face of dischordance of their biology. Our human mission is comfort, safety and reliability, with professionals valued for their commitment to mastery and human service and patients helped to find the meaning in their quality calculus.