
I read with dismay a recent announcement that as many as 34% of American physicians are considering leaving the profession in the next 10 years, and 16% will make some transition away from clinical practice in the next 12 months; remarkably similar data were also published in 2010 in the New England Journal of Medicine.
Both surveys came to the same conclusions: physicians are unhappy about their professional lives, and are extremely pessimistic about their futures. While economic burdens – costs more than income – are cited as a top reason, the bulk of their concerns related to their sense of control – or lack of it – over their professional identity and the role and place of physicians in emerging systems of care.

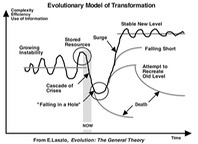
However, we are now at a moment in history where there is an extraordinary opportunity for physicians to recapture their leadership roles in patient care and the systems of care in which it takes place. If the operational systems and technology that are being imposed on us are flawed and less than optimal in design and functionality, that means there is an opportunity to actively determine the fate of what is likely to be an ‘intermediate species’ in the evolution of modern healthcare, and the professional of medicine has an incredibly powerful tool that we can, and must, employ to wrest control and drive the evolution of these systems: science.
So, please friends and colleagues: don’t go yet, the biggest opportunity of our careers is just opening up.
Medicine is the science of solving human problems, and success requires mastery of science, problem solving and humanness. We trusted in this model to give us the power to care for patients and we must trust in it to help us revitalize our roles as leaders in the healthcare system. A recent report issued by The Physicians Foundation spelled out our value very clearly: “Physicians and their relationship with patients constitute the animating principle of the US healthcare system”
Unfortunately, for most physicians today, the environments in which they work, whether in independent private practice or as organizational employees, are killing this vital spirit and undermining the very contribution physicians are expected to make to the success of the system. One of the fundamental requirements of the successful practice of medicine is the sense that your efforts – your studies, your discipline, your mastery, and your work of worry -- will be channeled to achieve some form of positive results for your patient and be valued by the community.
Health professionals take on an extraordinary depth of responsibility for other people’s lives; as
such, their confidence, optimism and professionalism must  be nurtured and cannot
survive in a vacuum. Our society seems
to understand the importance of this dynamic when it comes to the performance
of elite athletes, but we can’t seem to make the same respectful accommodations
to the critical performance of those we entrust with our health and our lives. But while “the system” today may not
adequately support the role of physician as central figure, an emerging set of
critical issues will place physicians, if we are organized enough to take advantage
of it, in a position of not only controlling our own destiny, but driving the
fundamental framework for “the system” itself.
be nurtured and cannot
survive in a vacuum. Our society seems
to understand the importance of this dynamic when it comes to the performance
of elite athletes, but we can’t seem to make the same respectful accommodations
to the critical performance of those we entrust with our health and our lives. But while “the system” today may not
adequately support the role of physician as central figure, an emerging set of
critical issues will place physicians, if we are organized enough to take advantage
of it, in a position of not only controlling our own destiny, but driving the
fundamental framework for “the system” itself.

Once upon a time, there were well defined, socially accepted modes of interaction between patients, health care professionals, and healthcare institutions. At a superficial level, patients accepted physician authority without question and in exchange, physicians would shoulder the whole work of worry about a patient’s health; while this model had its own flaws, it left the social structure of healthcare more certain. It was from this social compact – a balance of singular authority and mutual commitment — that patients felt they were able to move through difficult times with confidence.
While the paternalism of the old model is largely unacceptable in modern society, the model had a sense of wholeness and integrity that was comfortable and comforting to patients and community, providing a central figure — the physician — who accepted us in the face of imperfection, offering a professional form of unconditional love and its associated commitments.
Patients and the community are now
confronted with increasingly complex systems that are iterations of adaptations
to situations and circumstances – many of which began outside the realm of the
healthcare system – and often find themselves stranded without credible social
constructs for healthcare, often with fluctuating authority. The deconstruction of the culturally standardized healthcare structure has left us with a system that has no
rational base. The system has no evolutionary logic, nor could it pass even the
most superficial test of ‘evidence-based’.
standardized healthcare structure has left us with a system that has no
rational base. The system has no evolutionary logic, nor could it pass even the
most superficial test of ‘evidence-based’.
As a result, most people face major healthcare events with doubt and confusion.
Deconstruction of physician authority may have brought about broader individual awareness, but also systemic weaknesses; the physician community, vulnerable to competition for our social capital from forces who were unimpeded by the mores of academic and professional fairness that underlie our profession, fell victim to those with less selfless and less generous agendas, resulting in devaluation of our role.

Physicians started out the 21st century in a position of weakness; our leadership position was weakened, our professional judgment and competence questioned and our autonomy was under threat. The “health system” showed little interest in improving medical practice and took advantage of our vulnerability by offloading administrative responsibilities and offsetting costs to the physician community.

Over time, the ‘medical-business’ complex became a superficially dominant force, and we responded by organizing around our specialty identities and entering into a zero-sum game, where we bickered over how dollars are divided among ourselves while third-parties doled them out like parents deciding if we earned our allowance; this fragmentation, pitting physician-against-physician only served to weaken the profession even more as we tried to play a game whose rules were largely foreign to our professional culture, leaving us both unprepared and ambivalent.
Professional devaluation takes place on two levels: economic and social. For decades, physicians have reacted by been trying to fight the battle on someone else’s terms – economics – and trying to fight on other peoples terms is almost always a losing proposition. The key to our success is to shift the battlefield to one in which we dominate: the science of solving human problems.
 Why go into battle at all? Why not just quit; take our toys and go
home or give up on autonomy and become salaried employees? Well, first because of why we
became physicians in the first place:
our commitment to excellence and human service, and second, because,
actually, have a good chance of winning, both socially and economically. Society needs us, and we can do
well by doing good.
Why go into battle at all? Why not just quit; take our toys and go
home or give up on autonomy and become salaried employees? Well, first because of why we
became physicians in the first place:
our commitment to excellence and human service, and second, because,
actually, have a good chance of winning, both socially and economically. Society needs us, and we can do
well by doing good.
Two forces are in our favor. The first is the evolutionary
principle, as described by Nobel laureate Edmund O. Wilson that “while within groups,
selfish individuals beat altruistic individuals, groups of altruists (consistently) beat
groups of selfish  individuals”[1]. This means that if we organize around
and commit to our fundamentally altruistic professional mission, we will have a
better chance of winning the battle for our professional identity than if we
keep trying to compete on relatively selfish goals – like money.
individuals”[1]. This means that if we organize around
and commit to our fundamentally altruistic professional mission, we will have a
better chance of winning the battle for our professional identity than if we
keep trying to compete on relatively selfish goals – like money.
The second force in our favor is the free market. It is well
established that people will pay a premium for the delivery (and sometimes just the perception) of value; the
Ford Taurus you rent from Avis is exactly the same car you can get from Budget,
yet people show preferences and are  willing to pay a premium for one over the
other. By regaining control over
our professional identity, we also revalue ourselves in the marketplace.
willing to pay a premium for one over the
other. By regaining control over
our professional identity, we also revalue ourselves in the marketplace.
This defines our mission: revitalizing the value of the physician in the healthcare system. Rather than deploy our resources across multiple battlefields, we as a profession need to rally around a singular decisive infection point: redefining the foundational role of the physician, independent but inclusive of any and all specialty perspectives or competencies – medical, surgical, behavioral -- and reclaiming our profession.

Future of physicians is actually in a modern reclamation of three traditional roles:
- The determination of the value and significance of available information and how it should be applied to or removed from decisions – and actions -- that can affect the lives of human beings
- Serving as the orchestration point for plans of care by members of a patients’ professional and personal resource-communitie
- Take responsibility and shoulder the “work of worry” for the health and well being of our entire practice population, not just those who self-select for care but those who may have been in our waiting room recently.
There was a
time when physicians shouldered all the risk for patient care; we took care of
the patient and they either paid or they did not; if not, sometimes we took a
chicken. There was also a time
when physicians were the primary employers of nurses, who served critical roles
as care coordinators and care managers.
Physicians with better reputations garnered higher fees -- of course in
those days, patient satisfaction was not scored by Federal survey, but by how
neighbors talked about you in the supermarket. This is not a call to recover the past, but to remember that
our profession is familiar with some of these principles seemingly being
imposed on us.
So, at a
moment in the history of medicine when we are needed most to achieve the
broadest improvements in the health of our nation, it is time to activate ourselves. Let us: 
- Take a critical look at boundaries to a cohesive professional identity across medicine -- the things that evolved as defensive reactions to outside threats and, if they do not serve our vision for the future, bravely eliminate them.
- Adopt the emerging roles that suit our profession – knowledge manager, population view and conductor, and find the most relevant science to support our success in these roles.
- Wrest control of the strategies and frameworks for care delivery and determinations of quality that are infiltrating our professional lives, and set the standards against which products and systems are designed and operated.
 Let us reclaim our professional identity; let's lead with craftsmanship and relentless intellectual energy and the vigorous commitment to research and discovery that is the foundation of the profession to
which we aspired. The opportunity
exists for us to rewrite the script for our future and, in doing so, define our
leadership position and value to society.
Let us reclaim our professional identity; let's lead with craftsmanship and relentless intellectual energy and the vigorous commitment to research and discovery that is the foundation of the profession to
which we aspired. The opportunity
exists for us to rewrite the script for our future and, in doing so, define our
leadership position and value to society.
